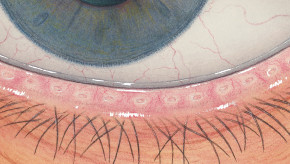
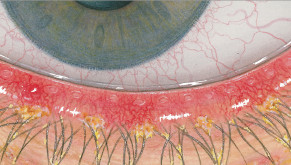
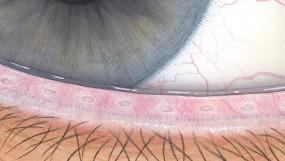
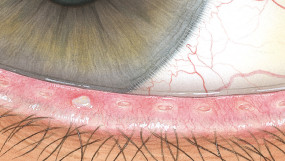
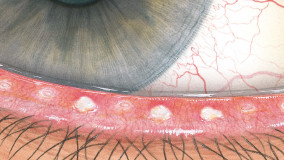
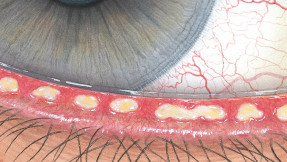
Blepharitis
Signs
Redness
Telangiectasis
Scaling of lid margins
brittle, leaving bleeding ulcer when removed
Lashes stuck together
Lash collarette
Madarosis
Poliosis
Tylosis
Telangiectasis
Scaling of lid margins
brittle, leaving bleeding ulcer when removed
Lashes stuck together
Lash collarette
Madarosis
Poliosis
Tylosis
Symptoms
Burning
Itching
Mild photophobia
Foreign body sensation
Dry eye - worse in morning
Lens intolerance
Itching
Mild photophobia
Foreign body sensation
Dry eye - worse in morning
Lens intolerance
Pathology
Staphylococcal endotoxin-induced complications include:
low grade conjunctivitis
toxic punctate epitheliopathy
low grade conjunctivitis
toxic punctate epitheliopathy
Aetiology
Staphylococcal infection of eyelash follicle
Treatment
Antibiotic ointments
Promote lid hygiene
Steroids
Artificial tears
May need to suspend lens wear during acute treatment phase
Promote lid hygiene
Steroids
Artificial tears
May need to suspend lens wear during acute treatment phase
Prognosis
Variable: expect periods of remission and exacerbation
Differential Diagnosis
Need to differentiate from seborrhoeic anterior blepharitis
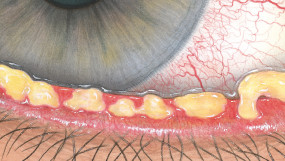
Meibomian gland dysfunction
Signs
Cloudy, creamy, yellow expression
Inspissated discharge
Poorly wetting lenses
Tear meniscus frothing
No secretion if blocked
Distended or distorted meibomian glands seen in retroillumination
Inspissated discharge
Poorly wetting lenses
Tear meniscus frothing
No secretion if blocked
Distended or distorted meibomian glands seen in retroillumination
Symptoms
Smeary vision
Greasy lenses
Dry eye
Lens intolerance
Greasy lenses
Dry eye
Lens intolerance
Pathology
MGD is a form of posterior blepharitis
Blocked meibomian orifice
Increased keratinisation of duct walls
Blocked meibomian orifice
Increased keratinisation of duct walls
Aetiology
Increased turnover of ductal epidermis
Abnormal meibomian oils
- more keratin proteins
Absence of lid rubbing
Abnormal meibomian oils
- more keratin proteins
Absence of lid rubbing
Treatment
Warm compresses
Heating devices
Lid scrubs/hygiene
Mechanical expression
Antibiotics
Tears/lipid supplements
Essential fatty acids
Sex hormones
Surfactant lens cleaning
Intraductal probing
Heating devices
Lid scrubs/hygiene
Mechanical expression
Antibiotics
Tears/lipid supplements
Essential fatty acids
Sex hormones
Surfactant lens cleaning
Intraductal probing
Prognosis
Excellent if good control can be achieved
Differential Diagnosis
External hordeolum
-localised swelling at lid margin
Internal hordeolum
-tender localised swelling
Chalazion
-chronic form of meibomian gland dysfunction
-localised swelling at lid margin
Internal hordeolum
-tender localised swelling
Chalazion
-chronic form of meibomian gland dysfunction
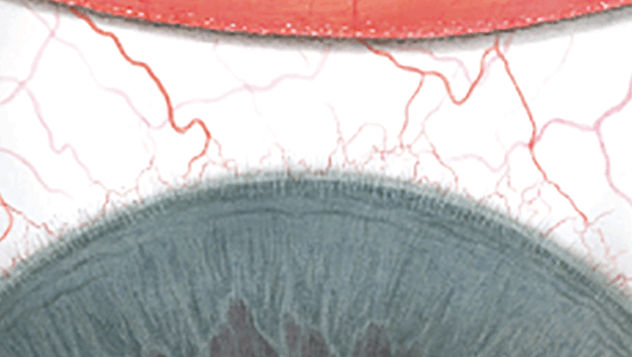
Superior limbic keratoconjunctivitis
Signs
Superior limbic redness
Infiltrates
Micropannus
Corneal staining
Conjunctival staining
Hazy epithelium
Papillary hypertrophy
Corneal filaments
Corneal warpage
Infiltrates
Micropannus
Corneal staining
Conjunctival staining
Hazy epithelium
Papillary hypertrophy
Corneal filaments
Corneal warpage
Symptoms
Lens awareness
Burning
Itching
Photophobia
Slight vision loss
- with extensive pannus
Burning
Itching
Photophobia
Slight vision loss
- with extensive pannus
Pathology
Cornea
-epitheliopathy
-infliltrates
Conjunctiva
-epithelial keratinization
-epithelial oedema
-inflammatory cells
-epitheliopathy
-infliltrates
Conjunctiva
-epithelial keratinization
-epithelial oedema
-inflammatory cells
Aetiology
Lens deposits
-posterior lens surface
Mechanical irritation
Immunological reaction
Hypoxia under lid
Thimerosal
-hypersensitivity
-toxicity
-posterior lens surface
Mechanical irritation
Immunological reaction
Hypoxia under lid
Thimerosal
-hypersensitivity
-toxicity
Treatment
Cease lens wear until inflammation subsides
Reduce wearing time
Improve solutions
Ocular lubricant
Mast cell stabilizers
Non-steroid anti-inflammatory agents
Increase frequency of lens replacement
Surgery if severe
Reduce wearing time
Improve solutions
Ocular lubricant
Mast cell stabilizers
Non-steroid anti-inflammatory agents
Increase frequency of lens replacement
Surgery if severe
Prognosis
After ceasing lens wear
-redness resolves rapidly
-epithelium resolves slowly
-can take from 3–40 weeks to resolve
-redness resolves rapidly
-epithelium resolves slowly
-can take from 3–40 weeks to resolve
Differential Diagnosis
Superficial epithelial arcuate lesion
-conjunctiva not involved
Bacterial conjunctivitis
Infiltrative keratitis
Theodore's superior limbic keratoconjunctivitis
-conjunctiva not involved
Bacterial conjunctivitis
Infiltrative keratitis
Theodore's superior limbic keratoconjunctivitis
Corneal infiltrates
Signs
Any condition whereby there are infiltrates in the cornea
Ranges from minute, barely-detectable infiltrate to full-blown corneal ulcer
Often used in the literature to denote a mild event
Ranges from minute, barely-detectable infiltrate to full-blown corneal ulcer
Often used in the literature to denote a mild event
Symptoms
Depends on severity
Ranges from asymptomatic to suicidal pain
Treat as suspected microbial keratitis if:
-patient is wearing contact lenses
-patient reports ocular discomfort
-infiltrates are observed in the uncomfortable eye
Ranges from asymptomatic to suicidal pain
Treat as suspected microbial keratitis if:
-patient is wearing contact lenses
-patient reports ocular discomfort
-infiltrates are observed in the uncomfortable eye
Pathology
Infiltrates in the epithelium and/or stroma
Infiltrates can include one or more of the following:
-polymorphonuclear leucocytes
-other inflammatory cells
-oedema
-microorganisms
By definition, Pseudomonas, Acanthamoeba and Fusarium keratitis are all CIEs
Infiltrates can include one or more of the following:
-polymorphonuclear leucocytes
-other inflammatory cells
-oedema
-microorganisms
By definition, Pseudomonas, Acanthamoeba and Fusarium keratitis are all CIEs
Aetiology
Varies: can be
-toxic
-allergic
-inflammatory
-traumatic
Risk factors:
-contaminated lenses
-solution inefficacy
-patient non-compliance
-poor hygiene
-hypoxia
-swimming
-overnight use
-overnight ortho-K
-mechanical trauma
-smoking
-diabetes
-warm climates
-male gender
-socio-economic class
-toxic
-allergic
-inflammatory
-traumatic
Risk factors:
-contaminated lenses
-solution inefficacy
-patient non-compliance
-poor hygiene
-hypoxia
-swimming
-overnight use
-overnight ortho-K
-mechanical trauma
-smoking
-diabetes
-warm climates
-male gender
-socio-economic class
Treatment
Depends on cause
Cease lens wear immediately
If discomfort persists after lens removal, scrape to test for offending microorganisms
Assume bacterial until proven otherwise:
-prescribe fluoroquinolones
Cold compresses
Analgesics
Continue appropriate treatment when scrape outcome is known
Avoid risk factors if lens wear is to resume
Cease lens wear immediately
If discomfort persists after lens removal, scrape to test for offending microorganisms
Assume bacterial until proven otherwise:
-prescribe fluoroquinolones
Cold compresses
Analgesics
Continue appropriate treatment when scrape outcome is known
Avoid risk factors if lens wear is to resume
Prognosis
Depends on cause; see various form of microbial keratitis below
-sterile CIEs may be self-limiting and resolve within 7 days
-microbial keratitis can rapidly progress to corneal perforation within hours
-sterile CIEs may be self-limiting and resolve within 7 days
-microbial keratitis can rapidly progress to corneal perforation within hours
Differential Diagnosis
Sterile vs microbial keratitis
Sterile keratitis is usually self-limiting
Microbial keratitis can advance rapidly
In the early stages, it is IMPOSSIBLE to differentially diagnose sterile vs microbial keratitis
Sterile keratitis is usually self-limiting
Microbial keratitis can advance rapidly
In the early stages, it is IMPOSSIBLE to differentially diagnose sterile vs microbial keratitis
Corneal ulcer
Signs
Small rounded peripheral ulcer
0.5 to 1 mm in diameter
Slight infiltration surrounding
There may be mild involvement of the anterior chamber
The ulcer and surrounding area may be stained with fluorescein
Limbic and bulbar redness
May be seen in patients who sleep in their lenses
0.5 to 1 mm in diameter
Slight infiltration surrounding
There may be mild involvement of the anterior chamber
The ulcer and surrounding area may be stained with fluorescein
Limbic and bulbar redness
May be seen in patients who sleep in their lenses
Symptoms
Eye redness
Tearing
Moderate to severe pain
Foreign body sensation
May be asymptomatic
The patient may report that they see a white spot on their eye
May show just after waking
Tearing
Moderate to severe pain
Foreign body sensation
May be asymptomatic
The patient may report that they see a white spot on their eye
May show just after waking
Pathology
Excavation focal epithelium
Background:
-Polymorphonuclear leukocytes (PMN)
Anterior stromal necrosis
Bowman's layer is intact
Background:
-Polymorphonuclear leukocytes (PMN)
Anterior stromal necrosis
Bowman's layer is intact
Aetiology
Toxins from gram-positive bacteria
Eye closure
Hypoxia
Eye closure
Hypoxia
Treatment
Remove the lens
Prescribe:
-fluoroquinolones
-Antibiotic ointment
Saline in single dose
Cold packs
Analgesics
Corticosteroid eyedrops
Fit 1 day lenses
Remove trauma
Improve maintenance regimen
Improve hygiene
Fit rigid lenses
Fit low water content lenses
Increase Dk/t
Prescribe:
-fluoroquinolones
-Antibiotic ointment
Saline in single dose
Cold packs
Analgesics
Corticosteroid eyedrops
Fit 1 day lenses
Remove trauma
Improve maintenance regimen
Improve hygiene
Fit rigid lenses
Fit low water content lenses
Increase Dk/t
Prognosis
Excellent:
-21% of cases resolve within 7 days
-All cases are resolved within 2-3 months
-21% of cases resolve within 7 days
-All cases are resolved within 2-3 months
Differential Diagnosis
Microbial keratitis
Viral epidemic keratoconjunctivitis:
-Typically bilateral
Stromal opacities
Stromal citcatrices
Viral epidemic keratoconjunctivitis:
-Typically bilateral
Stromal opacities
Stromal citcatrices
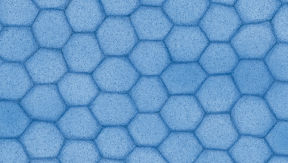
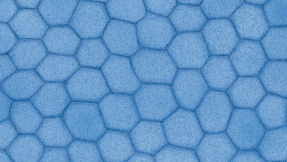
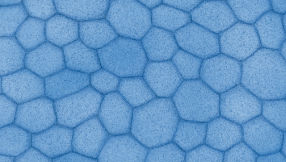
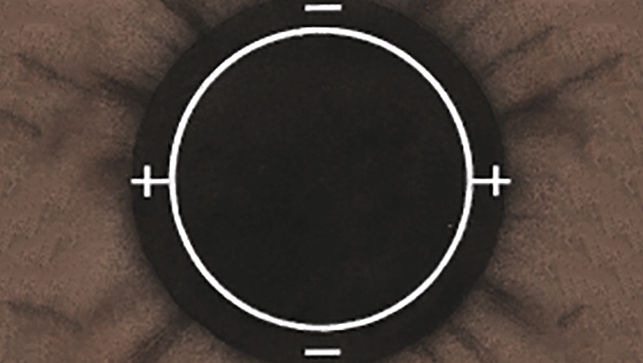
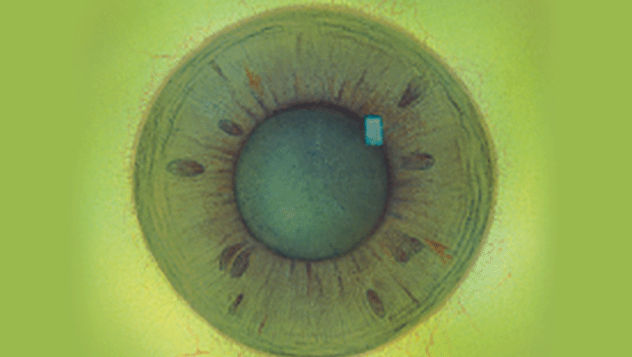
Endothelial polymegethism
Signs
Large variation in endothelial cell size
Small: large cell ratio:
-normal: 1 : 5
-polymegethism: 1 : 20
Small: large cell ratio:
-normal: 1 : 5
-polymegethism: 1 : 20
Symptoms
Asymptomatic
Corneal exhaustion syndrome:
-reduced wearing time
-discomfort
Corneal exhaustion syndrome:
-reduced wearing time
-discomfort
Pathology
Altered lateral cell walls
Straightening of interdigitations
Cell volume unchanged
Cell organelles normal
Poor oedema recovery
Straightening of interdigitations
Cell volume unchanged
Cell organelles normal
Poor oedema recovery
Aetiology
Acidic pH shift at endothelium due to
-hypercapnia: carbonic acid
-hypoxia: lactic acid
Chronic response
-hypercapnia: carbonic acid
-hypoxia: lactic acid
Chronic response
Treatment
General strategy
-alleviate acidosis
-higher Dk materials
Corneal exhaustion syndrome
-reduce wearing time
-fit higher Dk/t lens
-alleviate acidosis
-higher Dk materials
Corneal exhaustion syndrome
-reduce wearing time
-fit higher Dk/t lens
Prognosis
Possible long-term recovery (many years) after ceasing lens wear
Differential Diagnosis
Guttae
Endothelial dystrophy
Endothelial dystrophy
Endothelial blebs
Signs
Black non-reflecting areas
Apparent separation of cells
Apparent separation of cells
Symptoms
None
Pathology
Oedema of cell nucleus
Intracellular vacuoles
Extracellular vacuoles
Posterior surface bulging
Intracellular vacuoles
Extracellular vacuoles
Posterior surface bulging
Aetiology
Acidic pH shift at endothelium due to
-hypercapnia: carbonic acid
-hypoxia: lactic acid
Acute response
-hypercapnia: carbonic acid
-hypoxia: lactic acid
Acute response
Treatment
Not necessary
Prognosis
After inserting lens
-peak response in 10 min
-low level blebs continue
After removing lens
-disappear in 2 minutes
-peak response in 10 min
-low level blebs continue
After removing lens
-disappear in 2 minutes
Differential Diagnosis
Guttae
-permanent
Bedewing
-lasts months
Blebs
-last minutes
-permanent
Bedewing
-lasts months
Blebs
-last minutes
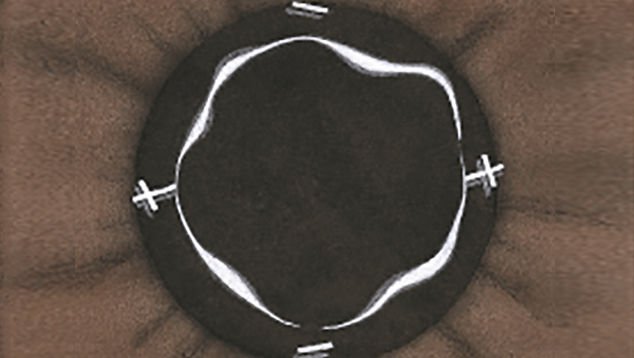
Corneal distortion
Signs
Can manifest as change in corneal:
-curvature
-symmetry
-regularity
Corneal indentation
-may be associated with corneal binding
-curvature
-symmetry
-regularity
Corneal indentation
-may be associated with corneal binding
Symptoms
Spectacle blur
Haze
-if associated with excess oedema
Haze
-if associated with excess oedema
Pathology
Surface Asymmetry Index
-more likely with rigid lenses
-decentred lens flattens cornea
Surface Regularity Index
-distortion may be symmetrical
-more likely with rigid lenses
Corneal indentation
-pressure from lens edge
-more likely with rigid lenses
-decentred lens flattens cornea
Surface Regularity Index
-distortion may be symmetrical
-more likely with rigid lenses
Corneal indentation
-pressure from lens edge
Aetiology
Oedema
-increased fluid
Physical moulding
-pressure from rigid lenses
-supplementary pressure from eyelids
Associated pathology, e.g. keratoconus
-increased fluid
Physical moulding
-pressure from rigid lenses
-supplementary pressure from eyelids
Associated pathology, e.g. keratoconus
Treatment
Alleviate rigid bearing
Alleviate hypoxia
Corneal indentation
-patient-dependent
-likely to recur again in same patient
Keratoplasty for keratoconus
Alleviate hypoxia
Corneal indentation
-patient-dependent
-likely to recur again in same patient
Keratoplasty for keratoconus
Prognosis
Rigid lens warpage
-full recovery in 5 to 8 months
Rigid lens binding
-full recovery in 24 hours
Soft lens warpage
-resolves in 7 days
-full recovery in 5 to 8 months
Rigid lens binding
-full recovery in 24 hours
Soft lens warpage
-resolves in 7 days
Differential Diagnosis
Keratoconus
-other signs present such as stromal thinning, Vogt’s striae and Fleischer’s ring
-other signs present such as stromal thinning, Vogt’s striae and Fleischer’s ring
Conjunctival redness
Signs
Conjunctival redness
May be regional variation
Specify location
Depends on lens type:
-no lens: grade 0.78
-rigid lens: grade 0.96
-soft lens: grade 1.54
May be regional variation
Specify location
Depends on lens type:
-no lens: grade 0.78
-rigid lens: grade 0.96
-soft lens: grade 1.54
Symptoms
Often none
Itchiness
Congestion
Warm feeling
Cold feeling
Non-specific mild irritation
Itchiness
Congestion
Warm feeling
Cold feeling
Non-specific mild irritation
Pathology
Vasodilatation due to:
-relaxation of smooth muscle
-vessel blockage
-relaxation of smooth muscle
-vessel blockage
Aetiology
Hypoxia & hypercapnia
Mechanical irritation
Immunological reaction
Infection
Inflammation
-acute red eye
Solution toxicity
Change in tonicity
Change in pH
Neural control
Mechanical irritation
Immunological reaction
Infection
Inflammation
-acute red eye
Solution toxicity
Change in tonicity
Change in pH
Neural control
Treatment
Remove cause
-see aetiology
Decongestants
If > grade 2 cease wear
-see aetiology
Decongestants
If > grade 2 cease wear
Prognosis
Excellent
-recovery from acute redness within hours
-recovery from chronic redness within 2 days
-recovery from acute redness within hours
-recovery from chronic redness within 2 days
Differential Diagnosis
Cease lens wear
-rapid resolution implicates lens wear
-slow resolution suggests other cause
‘Push test’:
-for conjunctival vs. scleral involvement
Haemorrhage
-redness between vessels
-rapid resolution implicates lens wear
-slow resolution suggests other cause
‘Push test’:
-for conjunctival vs. scleral involvement
Haemorrhage
-redness between vessels
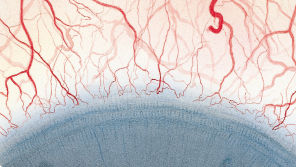
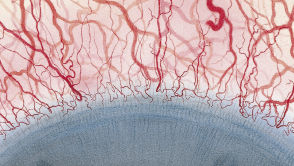
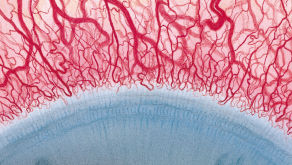
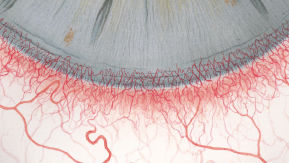
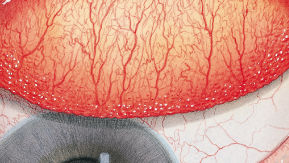
Limbal redness
Signs
Limbal redness
May be regional variation around limbus
Specify on record card
-virtually absent with silicone hydrogel lenses
May be regional variation around limbus
Specify on record card
-virtually absent with silicone hydrogel lenses
Symptoms
Depends on aetiology
-often none
-can be severe pain, e.g. with keratitis
Associated pathology may cause discomfort or pain
-often none
-can be severe pain, e.g. with keratitis
Associated pathology may cause discomfort or pain
Pathology
Vasodilatation of terminal arcades and associated vascular forms:
-recurrent limbal vessels
-vessel spikes
-recurrent limbal vessels
-vessel spikes
Aetiology
Hypoxia & hypercapnia
Mechanical irritation
Immunological reaction
Infection
Inflammation
-acute red eye
Solution toxicity
Mechanical irritation
Immunological reaction
Infection
Inflammation
-acute red eye
Solution toxicity
Treatment
Remove cause
-see aetiology
Consider whether:
-acute or chronic local limbal redness
-acute or chronic circumlimbal redness
Fit silicone hydrogel lenses
-see aetiology
Consider whether:
-acute or chronic local limbal redness
-acute or chronic circumlimbal redness
Fit silicone hydrogel lenses
Prognosis
Excellent
-recovery from acute redness within hours
-recovery from chronic redness within 2 days
-recovery from acute redness within hours
-recovery from chronic redness within 2 days
Differential Diagnosis
Re-vascularization
Vascularised limbal keratitis
Superior limbal keratoconjunctivitis
Vascularised limbal keratitis
Superior limbal keratoconjunctivitis
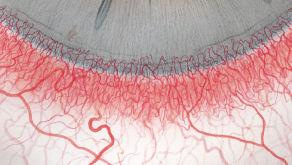
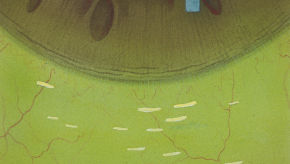
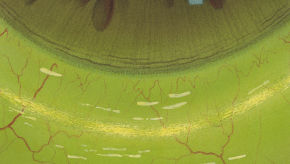
Corneal neovascularisation
Signs
Superficial vessels
-from conjunctiva
‘Normal’ responses:
-no lens: 0.2mm
-Silicone hydrogel: 0.2mm
-Daily wear hydrogel: 0.6mm
-Extended wear hydrogel: 1.4mm
-from conjunctiva
‘Normal’ responses:
-no lens: 0.2mm
-Silicone hydrogel: 0.2mm
-Daily wear hydrogel: 0.6mm
-Extended wear hydrogel: 1.4mm
Symptoms
No discomfort
Vision loss if extreme
Vision loss if extreme
Pathology
Sprouting or budding
Solid cord of vascular endothelial cells at growing tip
Thin vessel wall
Pericytes
Cell migration
Surrounding inflammatory cells
Disruption of stromal lamellae
Lipid material may surround vessels
Solid cord of vascular endothelial cells at growing tip
Thin vessel wall
Pericytes
Cell migration
Surrounding inflammatory cells
Disruption of stromal lamellae
Lipid material may surround vessels
Aetiology
Stromal softening
-hypoxia-induced oedema
Triggering agent, e.g.:
-epithelial damage
-solution toxicity
-infection
-hypoxia-induced oedema
Triggering agent, e.g.:
-epithelial damage
-solution toxicity
-infection
Treatment
If severe
-cease lens wear permanently
If mild
-improve care system
-increase Dk/t
-reduce wearing time
-monitor carefully
-cease lens wear permanently
If mild
-improve care system
-increase Dk/t
-reduce wearing time
-monitor carefully
Prognosis
On ceasing lens wear
-vessels empty rapidly
-ghost vessels remain
-years to resolve
On reintroducing lens
-ghost vessels rapidly refill
-vessels empty rapidly
-ghost vessels remain
-years to resolve
On reintroducing lens
-ghost vessels rapidly refill
Differential Diagnosis
Nerve fibres
-any orientation
-’solid’
Striae
-always vertical
-white, whispy
Ghost vessels
-start at limbus
-relatively thick
-any orientation
-’solid’
Striae
-always vertical
-white, whispy
Ghost vessels
-start at limbus
-relatively thick
Epithelial microcysts
Signs
Minute scattered dots
Spherical or ovoid shape
5–30µm diameter
Reversed illumination
Spherical or ovoid shape
5–30µm diameter
Reversed illumination
Symptoms
Can cause slight discomfort
Can reduce vision slightly
Can reduce vision slightly
Pathology
Intraepithelial sheets
Disorganised cell growth
Pockets of dead cells
Slowly pushed to surface
Disorganised cell growth
Pockets of dead cells
Slowly pushed to surface
Aetiology
Possible factors:
-prolonged hypoxia
-mechanical irritation
-reduced oxygen uptake
-reduced mitosis
-typically hydrogel extended wear
-prolonged hypoxia
-mechanical irritation
-reduced oxygen uptake
-reduced mitosis
-typically hydrogel extended wear
Treatment
If ≤ grade 2 microcysts
-no action
-monitor carefully
If ≥ grade 3 microcysts
-cease wear (1 month)
-reduce wearing time
-change to daily wear
-increase lens Dk/t
-no action
-monitor carefully
If ≥ grade 3 microcysts
-cease wear (1 month)
-reduce wearing time
-change to daily wear
-increase lens Dk/t
Prognosis
After ceasing wear
-increase during first 7 days
-decrease thereafter
Full recovery in 2 months
Microcysts will not recur with silicone hydrogel lenses
-increase during first 7 days
-decrease thereafter
Full recovery in 2 months
Microcysts will not recur with silicone hydrogel lenses
Differential Diagnosis
Tear film debris
-move on blink
Mucin balls
Vacuoles
-unreversed optics
Bullae
Bedewing
-endothelial
Dimple veiling
-very large
-move on blink
Mucin balls
Vacuoles
-unreversed optics
Bullae
Bedewing
-endothelial
Dimple veiling
-very large
Corneal oedema
Signs
EPITHELIAL OEDEMA
Slight haziness of epithelium seen in optic section
Can occur during adaptation to rigid lens wear
STROMAL OEDEMA
<2% oedema: undetectable; safe
>5% oedema: vertical striae; caution
>8% oedema: posterior folds; danger
>15% oedema: loss of corneal transparency; pathological
Slight haziness of epithelium seen in optic section
Can occur during adaptation to rigid lens wear
STROMAL OEDEMA
<2% oedema: undetectable; safe
>5% oedema: vertical striae; caution
>8% oedema: posterior folds; danger
>15% oedema: loss of corneal transparency; pathological
Symptoms
EPITHELIAL OEDEMA
Asymptomatic
Appearance of haloes
STROMAL OEDEMA
<10% oedema: none
>10% oedema: discomfort
Asymptomatic
Appearance of haloes
STROMAL OEDEMA
<10% oedema: none
>10% oedema: discomfort
Pathology
EPITHELIAL OEDEMA
Disruption to epithelial cells
Extracellular oedema around basal epithelial cells
STROMAL OEDEMA
Oedema
-increased fluid
Striae
-separated collagen fibrils
Folds
-physical buckling
Disruption to epithelial cells
Extracellular oedema around basal epithelial cells
STROMAL OEDEMA
Oedema
-increased fluid
Striae
-separated collagen fibrils
Folds
-physical buckling
Aetiology
EPITHELIAL OEDEMA
Hypotonic tears, as occurs during lacrimation
Adaptation to rigid lens wear
Fluid enters epithelium
Fluid forms between basal epithelial cells
STROMAL OEDEMA
Primarily hypoxia – 50%
-lactate build-up
Other factors – 50%:
-tear hypotonicity
-hypercapnia
-increased temperature
-increased humidity
-mechanical
Hypotonic tears, as occurs during lacrimation
Adaptation to rigid lens wear
Fluid enters epithelium
Fluid forms between basal epithelial cells
STROMAL OEDEMA
Primarily hypoxia – 50%
-lactate build-up
Other factors – 50%:
-tear hypotonicity
-hypercapnia
-increased temperature
-increased humidity
-mechanical
Treatment
EPITHELIAL OEDEMA
Modify rigid lens adaptation wear regimen
STROMAL OEDEMA
Alleviate hypoxia
-increase material Dk
-reduce lens thickness
-increase lens movement
-increase edge lift
Alleviate hypercapnia
-as per hypoxia
Modify rigid lens adaptation wear regimen
STROMAL OEDEMA
Alleviate hypoxia
-increase material Dk
-reduce lens thickness
-increase lens movement
-increase edge lift
Alleviate hypercapnia
-as per hypoxia
Prognosis
EPITHELIAL OEDEMA
Rapid recovery upon ceasing of hypotonic stress, i.e. when tearing stops
STROMAL OEDEMA
Acute oedema
-resolves in 2-3 hours
Chronic oedema
-resolves in 7 days
Chronic oedema thins stroma
Rapid recovery upon ceasing of hypotonic stress, i.e. when tearing stops
STROMAL OEDEMA
Acute oedema
-resolves in 2-3 hours
Chronic oedema
-resolves in 7 days
Chronic oedema thins stroma
Differential Diagnosis
EPITHELIAL OEDEMA
Generalised epitheliopathy
STROMAL OEDEMA
Striae
-nerve fibres
-ghost vessels
Folds
-seen in diabetes
Haze
-scarring
-epithelial oedema
Generalised epitheliopathy
STROMAL OEDEMA
Striae
-nerve fibres
-ghost vessels
Folds
-seen in diabetes
Haze
-scarring
-epithelial oedema
Corneal staining
Signs
3 & 9 O’CLOCK CORNEAL STAINING
Punctate or diffuse staining at the 3&9 o’clock limbal locations
Triangular patterns:
-apex away from central cornea
-‘base’ corresponds to lens edge
-only seen in rigid lens wearers
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Inferior arcuate stain parallel to limbus
Punctate form
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Superior arcuate stain parallel to limbus
Full thickness lesion
Also known as ‘epithelial splitting’
Punctate or diffuse staining at the 3&9 o’clock limbal locations
Triangular patterns:
-apex away from central cornea
-‘base’ corresponds to lens edge
-only seen in rigid lens wearers
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Inferior arcuate stain parallel to limbus
Punctate form
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Superior arcuate stain parallel to limbus
Full thickness lesion
Also known as ‘epithelial splitting’
Symptoms
3 & 9 O’CLOCK CORNEAL STAINING
Slight discomfort
Dryness
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Slight discomfort
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Asymptomatic
Slight discomfort
Dryness
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Slight discomfort
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Asymptomatic
Pathology
3 & 9 O’CLOCK CORNEAL STAINING
Epithelial disruption at limbus
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Disruption to epithelium
Cells damaged or dislodged
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Full thickness splitting of epithelium
Epithelial disruption at limbus
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Disruption to epithelium
Cells damaged or dislodged
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Full thickness splitting of epithelium
Aetiology
3 & 9 O’CLOCK CORNEAL STAINING
Rigid lens bridges lid away from ocular surface
Ocular surface adjacent to lens edge not properly wetted
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Metabolic
Desiccation
-insufficient post-lens tear film
-lens adherence
-lens dehydration
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Mechanical chafing of superior cornea
Inward pressure of upper lid
Contributing factors:
-corneal topography
-rigid lens modulus
-mid-peripheral lens design
-lens surface
Rigid lens bridges lid away from ocular surface
Ocular surface adjacent to lens edge not properly wetted
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Metabolic
Desiccation
-insufficient post-lens tear film
-lens adherence
-lens dehydration
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Mechanical chafing of superior cornea
Inward pressure of upper lid
Contributing factors:
-corneal topography
-rigid lens modulus
-mid-peripheral lens design
-lens surface
Treatment
3 & 9 O’CLOCK CORNEAL STAINING
Alter lens design
-reduce thickness of lens edge
-smaller lens diameter
Blinking instructions
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Alter lens fit
-more movement
-thicker lens
Alter lens type
-different material
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Alter lens design
-less mid-peripheral bearing
Alter lens type
-lower modulus material
-better surface characteristics
Alter lens design
-reduce thickness of lens edge
-smaller lens diameter
Blinking instructions
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Alter lens fit
-more movement
-thicker lens
Alter lens type
-different material
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Alter lens design
-less mid-peripheral bearing
Alter lens type
-lower modulus material
-better surface characteristics
Prognosis
3 & 9 O’CLOCK CORNEAL STAINING
Following lens removal
-recovery: <24 hours
While wearing lenses
-slower recovery: 4–5 days
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Following lens removal
-rapid recovery: <24hours
While wearing lenses
-slower recovery: 4-5 days
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Following lens removal
-recovery in 3 days
Following lens removal
-recovery: <24 hours
While wearing lenses
-slower recovery: 4–5 days
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Following lens removal
-rapid recovery: <24hours
While wearing lenses
-slower recovery: 4-5 days
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Following lens removal
-recovery in 3 days
Differential Diagnosis
3 & 9 O’CLOCK CORNEAL STAINING
Vascularised limbal keratitis
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Lens edge stain
Lens insertion/removal trauma
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Lens edge stain
Lens insertion & removal trauma
Vascularised limbal keratitis
INFERIOR EPITHELIAL ARCUATE LESION ('SMILE STAIN')
Lens edge stain
Lens insertion/removal trauma
SUPERIOR EPITHELIAL ARCUATE LESION (SEAL)
Lens edge stain
Lens insertion & removal trauma
Conjunctival staining
Signs
Normal eye: curved lines of staining in conjunctiva parallel to limbus; furrow staining
Lens-wearing eye:
-diffuse stain
-coalescent stain
-‘lens edge’ stain
Lens-wearing eye:
-diffuse stain
-coalescent stain
-‘lens edge’ stain
Symptoms
Often none
‘Lens edge’ stain may be associated with ‘tight lens syndrome’
‘Lens edge’ stain may be associated with ‘tight lens syndrome’
Pathology
Normal eye
-fluorescein pools in natural conjunctival folds
Lens-wearing eye
-superficial epithelial cells traumatised or dislodged
-fluorescein pools in natural conjunctival folds
Lens-wearing eye
-superficial epithelial cells traumatised or dislodged
Aetiology
‘Lens edge’ stain caused by physical trauma of lens edge
Diffuse stain due to other physical trauma
-trauma induced by excessive movement of loose fitting lens
Diffuse stain due to other physical trauma
-trauma induced by excessive movement of loose fitting lens
Treatment
‘Lens edge’ stain:
-fit flatter lens
Lens trauma stain:
-improve care regimen to alleviate deposit formation
-improve lens fit
-fit flatter lens
Lens trauma stain:
-improve care regimen to alleviate deposit formation
-improve lens fit
Prognosis
Excellent
-recovery within 2–4 days
-recovery within 2–4 days
Differential Diagnosis
Physiological ‘furrow staining’ vs. pathological staining
Papillary conjunctivitis
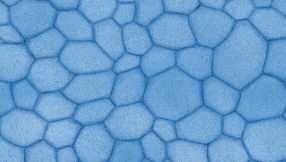
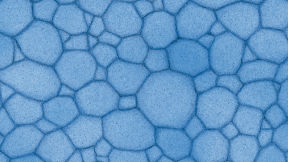
Signs
Papillae on tarsal conjunctiva
-‘cobblestone’ appearance
-‘giant’ papillae uncommon
Conjunctival redness
Conjunctival oedema
Excess lens movement
Coated contact lens
Mucus discharge
-‘cobblestone’ appearance
-‘giant’ papillae uncommon
Conjunctival redness
Conjunctival oedema
Excess lens movement
Coated contact lens
Mucus discharge
Symptoms
Early – grades 1&2
-lens awareness
-mild itching
-slight blur
Late – grades 3&4
-lens discomfort
-intense itching
-blur
-reduce wearing time
-lens awareness
-mild itching
-slight blur
Late – grades 3&4
-lens discomfort
-intense itching
-blur
-reduce wearing time
Pathology
Thickened conjunctiva
Distorted epithelial cells
Altered goblet cells
Inflammatory cells
-mast cells
-eosinophils
-basophils
Distorted epithelial cells
Altered goblet cells
Inflammatory cells
-mast cells
-eosinophils
-basophils
Aetiology
Lens deposits
-anterior lens surface
Mechanical irritation
Immunological reaction
Hypoxia under lid
Solution toxicity
-thimerosal
May be related to meibomian gland dysfunction
-anterior lens surface
Mechanical irritation
Immunological reaction
Hypoxia under lid
Solution toxicity
-thimerosal
May be related to meibomian gland dysfunction
Treatment
Cease lens wear until inflammation subsides
Reduce wearing time
Improve solutions
Ocular lubricant
Mast cell stabilisers
Non-steroid anti-inflammatory agents
Change to a lens material that deposits differently
Increase frequency of lens replacement
Improve ocular hygiene
Reduce wearing time
Improve solutions
Ocular lubricant
Mast cell stabilisers
Non-steroid anti-inflammatory agents
Change to a lens material that deposits differently
Increase frequency of lens replacement
Improve ocular hygiene
Prognosis
Papillae can remain for weeks, months or years
Lenses can still be worn
Treat according to symptoms
Lenses can still be worn
Treat according to symptoms
Differential Diagnosis
Follicle
-vessels on outside
Papilla
-central vascular tuft
-vessels on outside
Papilla
-central vascular tuft
This content is based on the book: CONTACT LENS COMPLICATIONS, Author NATHAN EFRON Ed: Butterworth-Heinemann, 1999.
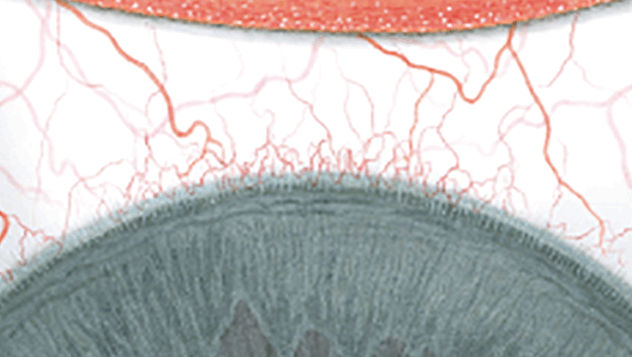
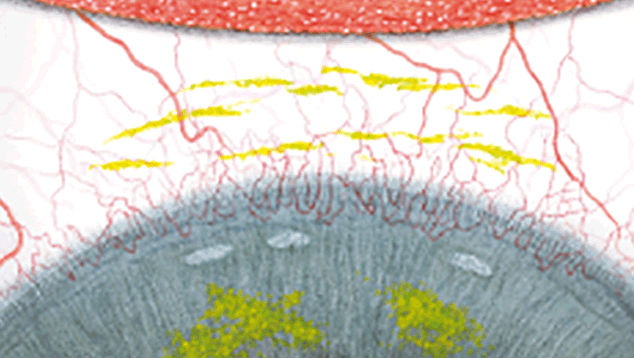
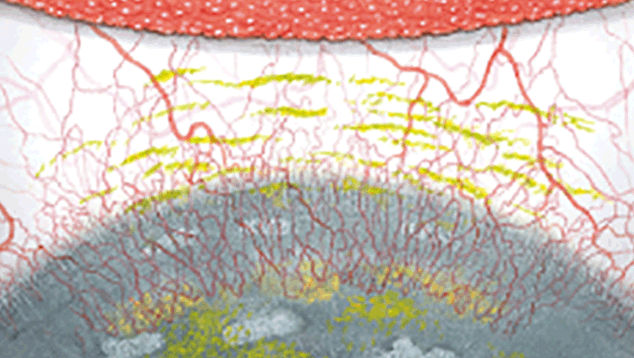
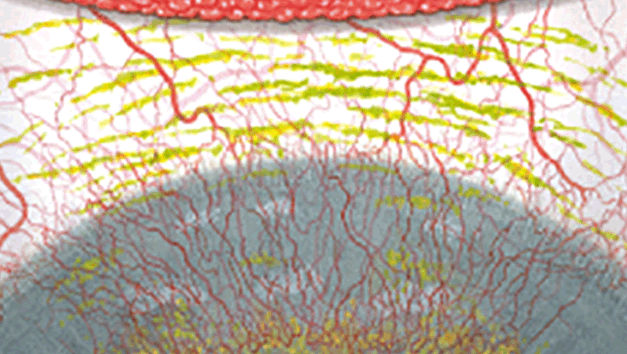
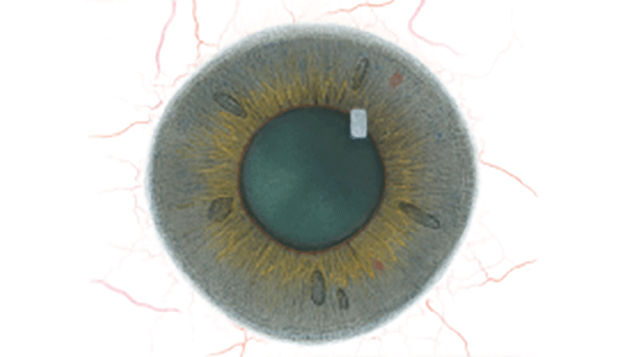
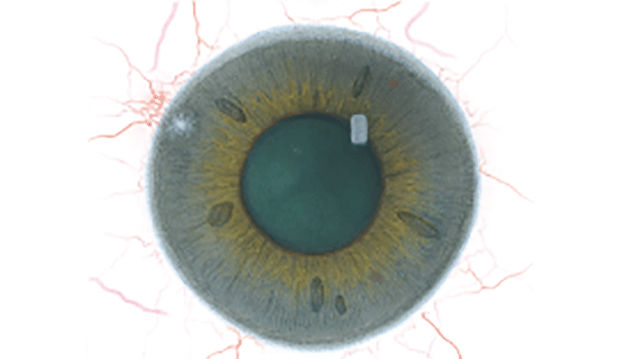
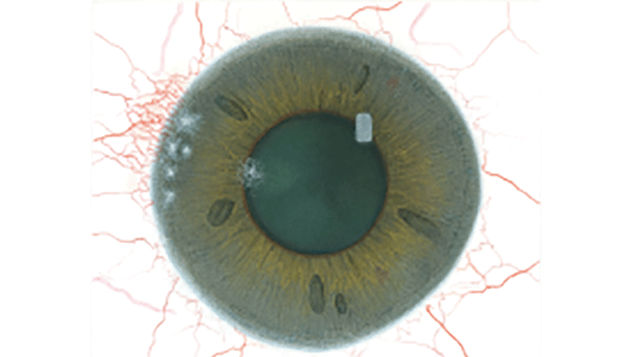
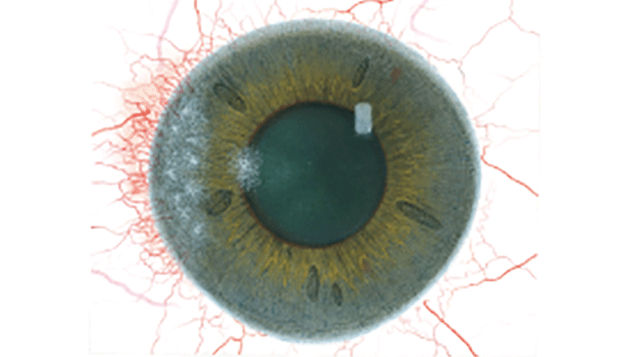
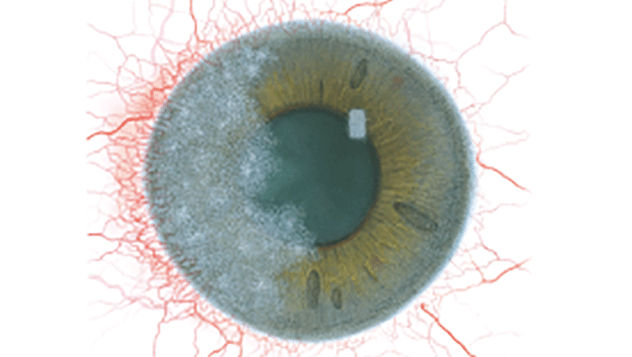
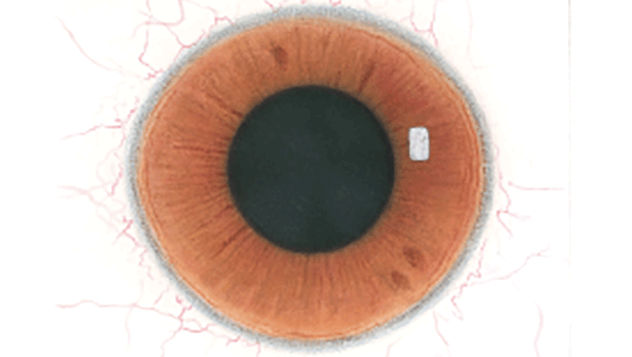
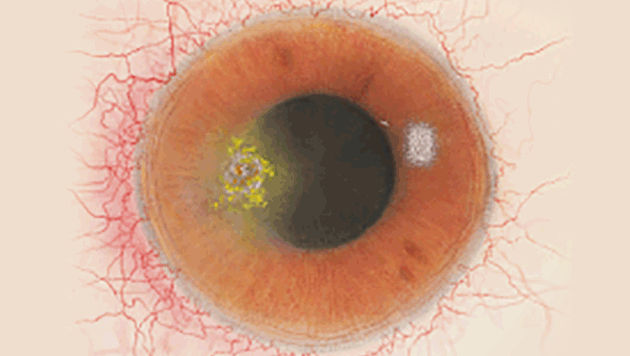
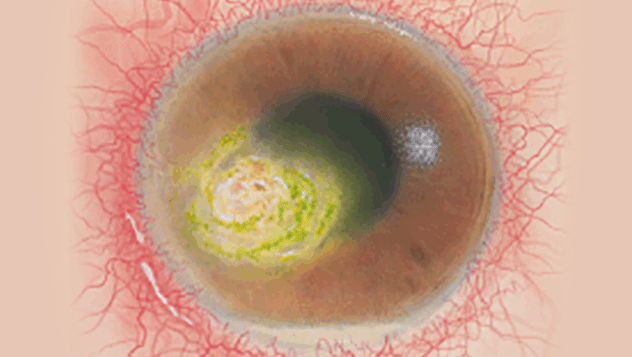
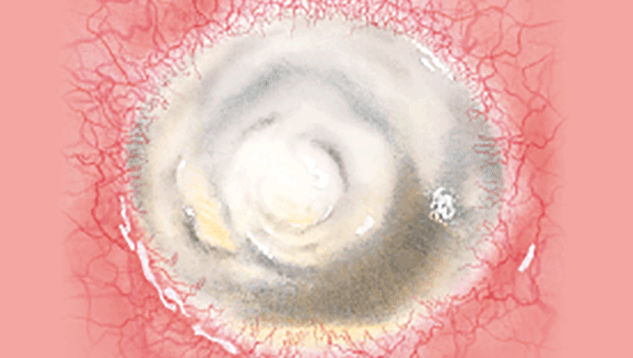
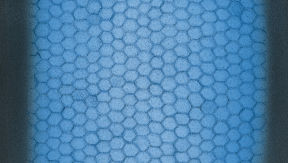
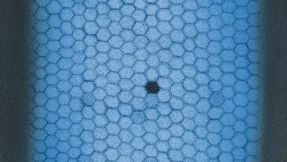
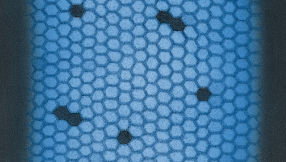
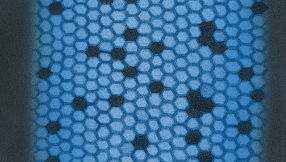
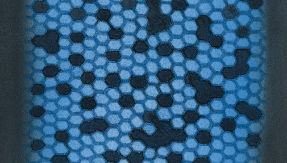
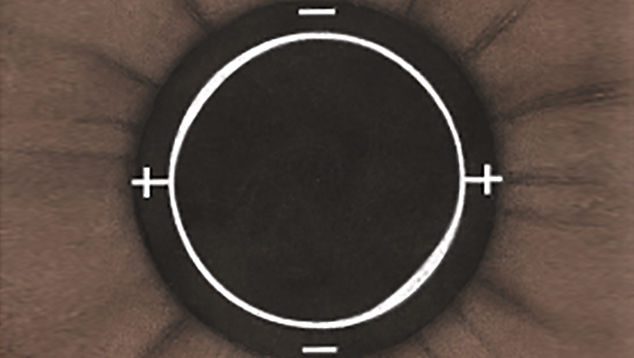
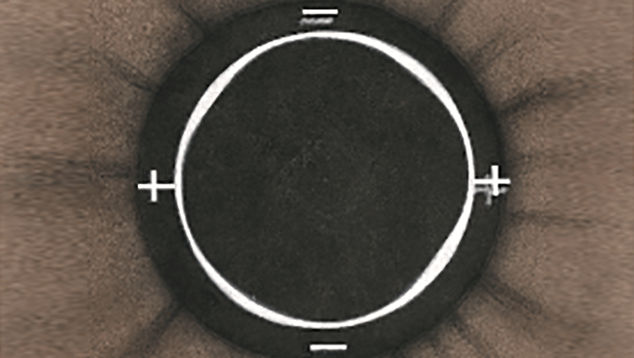
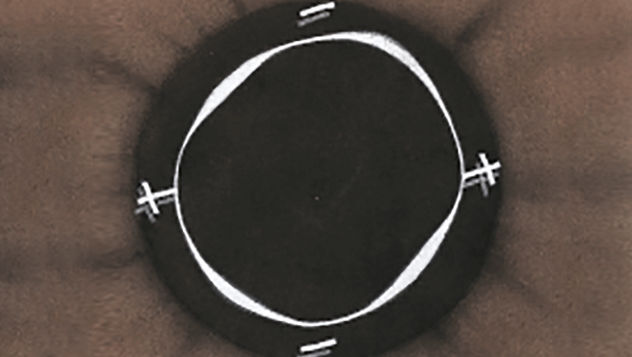
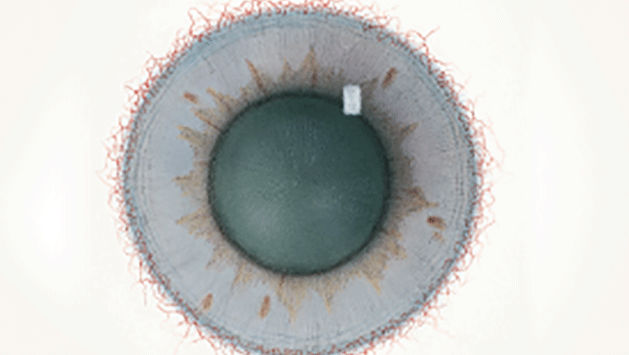
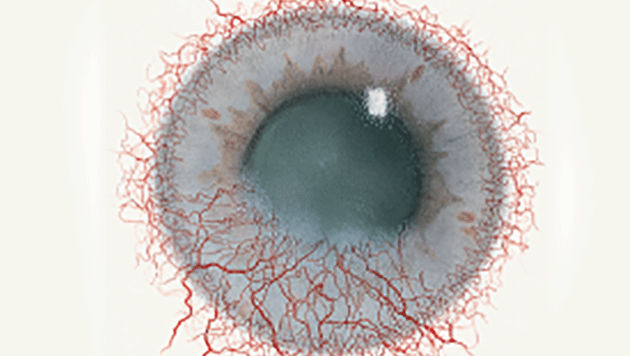
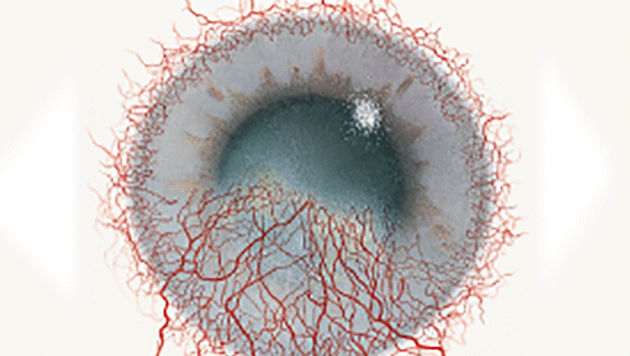
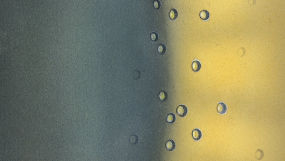
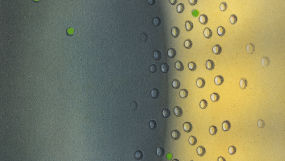
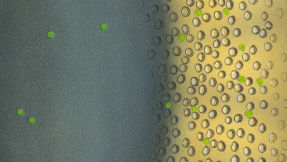
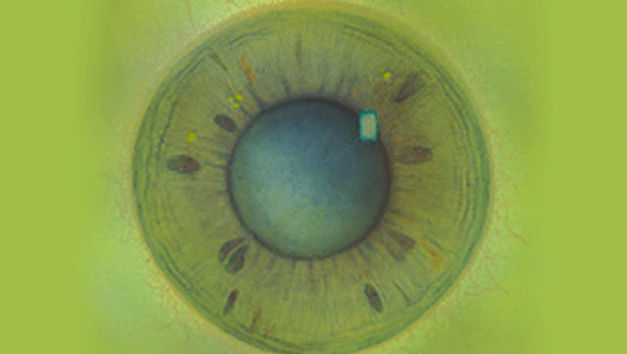
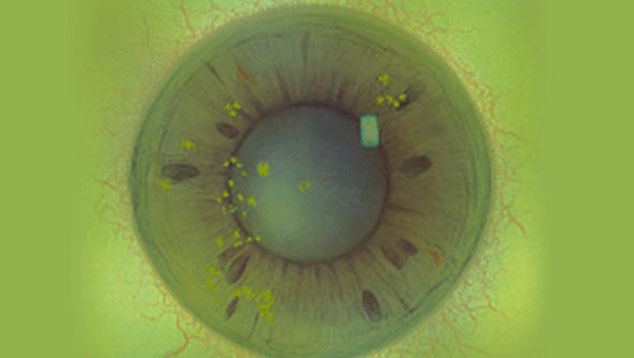
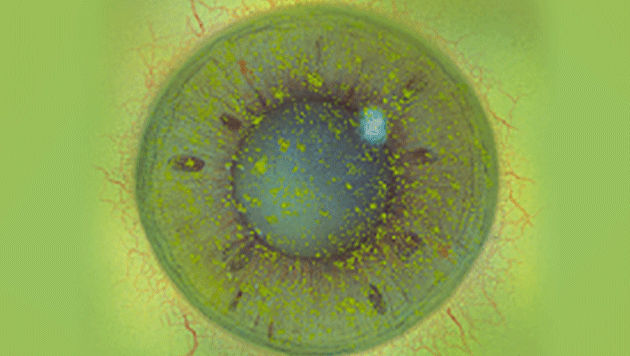
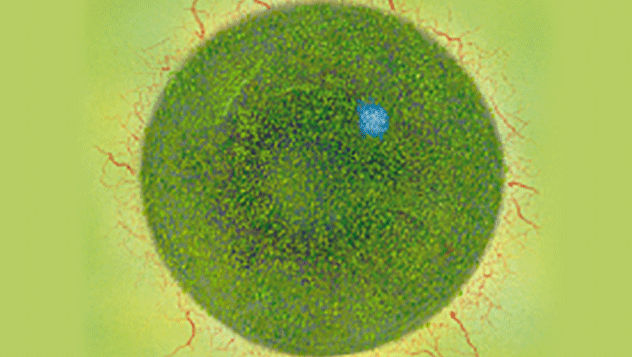
The Efron Grading Scales* provide a convenient clinical reference for eye care professionals.
On a scale of 0 to 4, it describes the severity of the following anterior ocular complications that can occur from contact lens wear.
- Meibomian gland dysfunction
- Superior limbic keratoconjunctivitis
- Corneal infiltrates
- Corneal ulcer
- Endothelial polymegethism
- Endothelial blebs
- Corneal distortion
- Conjunctival redness
- Limbal redness
- Corneal neovascularisation
- Epithelial microcysts
- Corneal oedema
- Corneal staining
- Conjunctival staining
- Papillary conjunctivitis
Each condition includes five illustrations. Simply select a number on the scale for the corresponding illustration and visual signs of severity. Select the Info button for symptoms, pathology, treatment options and more.
* The Efron Grading Scales are designed to help eye care practitioners. It is not a substitute for a professional consultation with a qualified eye care practitioner.